The procedure, known as Selective Internal Radiation Therapy (SIRT), uses the SIR-spheres microspheres (yttrium-90 resin microspheres) as an innovative form of internal radiotherapy for removing liver cancers. The yttrium-90 resin microspheres are inserted through the hepatic artery that feeds the vessel of the tumour. This goes directly to the affected area and dissolves the cancerous tumour or reduces it in size, without damaging the tissues surrounding the liver. This form of liver radiotherapy has been shown to be effective in treating patients with different forms of inoperable liver tumours.
The procedure is usually done once and will be effective in the patient’s system for about two weeks. The patient is required to go back to the hospital after three months for a check-up and monitoring of the progress.
Over 5 000 patients are diagnosed with colorectal cancer in South Africa annually. In over 40% of colorectal cancer patients, the disease will spread to the liver and cannot be removed surgically.
In addition, around 3 500 South African patients are diagnosed with primary liver cancer every year and approximately 85% of these are inoperable. Patients with inoperable liver tumours often have a poor prognosis even when treated with modern systemic chemotherapy and/or biological agents.
Professor Mike Sathekge, Head of the Department of Nuclear Medicine, said, “Selective Internal Radiation Therapy in the form of yttrium-90 resin microspheres is an exciting innovative radiation treatment for patients with inoperable liver tumours and we are very proud to be the first hospital in South Africa to introduce this form of treatment. The availability of this innovative radioembolisation therapy means new treatment options for patients, and advances in healthcare for the South African public.’’
“There is a growing interest in SIRT using yttrium-90 resin microspheres for the treatment of patients with liver metastases or with primary liver cancer. There is now substantial clinical evidence in comparative studies that SIRT in the form of SIR-spheres microspheres is an effective and well-tolerated therapy for treating patients with previously treated liver metastases from colorectal cancer. There is also mounting evidence that SIRT is an effective and well-tolerated treatment for inoperable primary liver cancer,” added Prof Sathekge.
He acknowledged the fact that the procedure would benefit the poor at an academic hospital and would also enhance a level of monitoring and improved research. He also said that the procedure prolongs the lifespan of cancer patients by three times. “Its location in a university hospital is perfect, where a multidisciplinary team of doctors will manage it and also monitor the progress made by a patient,” commented Prof Sathekge.
SIR-spheres microspheres are mainly used in Australia, the European Union, Switzerland, Turkey and several other countries including in Asia (eg India, Korea, Singapore and Hong Kong) for the treatment of inoperable liver tumours.
The Chief Executive Officer at the Steve Biko Academic Hospital, Dr Ernest Kenoshi, said the procedure might cost about R120 000 in a private hospital, but in the public sector patients would have to undergo an assessment to determine their fees. The poorest of the poor would, however, get the treatment at no cost. He said placing the therapy in a public hospital increases its accessibility to the general public, especially the poorest of the poor.
“This treatment is not for monetary gain, but for the benefit of patients and also for the advancement of healthcare in South Africa,” said Dr Kenoshi.
The Dean of the Faculty of Health Sciences at the University of Pretoria, Prof Eric Buch, lauded the new procedure and attributed it to the close partnership between the University of Pretoria and the Gauteng Department of Health. He said the relationship was pivotal in achieving the following three broad goals:
-
to bring an excellent quality healthcare to the poor people of South Africa,
-
to train outstanding health professionals, and
-
to produce relevant research in the country, and to bring new technologies and opportunities for healthcare to the people.
Prof Buch added that people from around the country and the continent are receiving high-quality treatment at the Steve Biko Academic Hospital, and this is because of high-quality care enriched by the partnership the hospital has with the University of Pretoria.
“The University of Pretoria and the Steve Biko Academic Hospital are able to attract outstanding doctors and other health professionals who are committed to patients’ care, and also committed to their educational purpose. This is reflected by Prof Sathekge’s work,” said Prof Buch.

At the press conference were Prof Mike Sathekge, Head of the Department of Nuclear Medicine, Dr Ernest Kenoshi, CEO of Steve Biko Academic Hospital, Prof Eric Buch, Dean of Faculty of Health Sciences at UP and Dr M Mathebula, Deputy CEO of Steve Biko Academic Hospital.
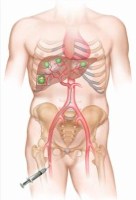
Picture 1: The yttrium-90 resin microspheres are introduced via a catheter inserted into the hepatic artery found in the groin. The catheter is pushed up to the liver until it reaches the exact spot where the tumour is (green balls on the liver). This targets only the tumour without damaging the surrounding tissues of the liver.
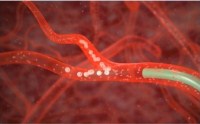
Picture 2: This is how yttrium-90 resin microspheres move into the vessel feeding the tumour.

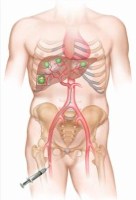
Picture 3: The tumours found on the liver will then shrink in size and eventually be destroyed.


Get Social With Us
Download the UP Mobile App